- Sports Med U Newsletter
- Posts
- Manual therapy + Exercise VS Corticoid Injections for patients with sub acromial pain | What is better?
Manual therapy + Exercise VS Corticoid Injections for patients with sub acromial pain | What is better?
Sports Med U | Educating Minds, Elevating Potential
Manual Therapy and Exercise Have Similar Outcomes to Corticosteroid Injections in the Management of Patients With Sub-acromial Pain Syndrome: A Systematic Review and Meta- Analysis
Karanasios, S., Baglatzis, G., Lignos, I., Billis, E. and Mpaglatzis, G., 2023. Manual Therapy and Exercise Have Similar Outcomes to Corticosteroid Injections in the Management of Patients With Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis. Cureus, 15(11).
In today’s letter
Overview of manual therapy + exercise and Corticoid-steroid injections effects on patient pain/discomfort
Rapid Results = Physiotherapy is just as effective as corticoid-steroid injections in short, medium & long term
Professional takeaway = Corticoid injections should only be considered if conservative treatment has no affects after 12-24 weeks
Bite-size study - Infographic style!

Whats new is SportsMed U
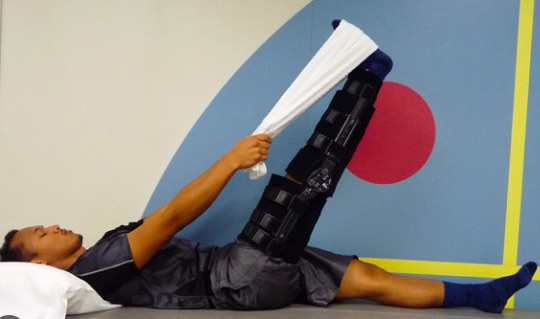
We are continuing our exploration of ACL and their physiotherapy management. This weeks article explains 6 key areas to focus on in early rehab post ACL reconstruction
Deeper look
Aim of study
This review aims to evaluate the effectiveness of a multimodal treatment approach, including manual therapy + exercise (EMT) compared with corticosteroid injections, in managing Subacromial pain syndrome (SAPS) across different follow-up times: very short-term (≤2 months), short-term (>2 months to ≤3 months), mid-term (>3 to <12 months), and long-term (⩾12 months).
Synthesise evidence on interventions, considering factors such as type, mode, frequency, etc., and follow an established approach to assess the certainty of evidence.
Background info
SAPS, also known as shoulder impingement syndrome, is the prevailing diagnosis for shoulder pain, observed in 11 to 12 cases per 1000 general practice consultations.
The lifetime prevalence of SAPS ranges from 7% to 26% in the general population, with an escalation tied to advancing age.
Pathogenesis involves multiple structures: Acromion, rotator cuff tendons, acromioclavicular joint, glenohumeral ligaments, and capsule. Read an explanation HERE

Clinical presentation includes pain, diminished shoulder movement, and impaired function during elevation and external rotation.
Published guidelines exhibit inconsistent recommendations for optimal SAPS management.
Common nonsurgical interventions encompass multimodal physiotherapy (including exercise and manual therapy - EMT) or corticosteroid injections.
Studies indicate EMT's significant improvement in SAPS patients, but the full extent of its effectiveness remains unclear.
Corticosteroid injections, widely used to mitigate SAPS-related inflammation, face debate regarding their overall efficacy.
Older reviews suggest corticosteroid injections yield short-term pain reduction, comparable to physiotherapy or placebo; however, no apparent advantages persist in mid- to long-term follow-ups.
Comprehensive understanding of SAPS and its management is critical, given the complex nature of the condition.


Methods
Inclusion Criteria:
Eligible participants are individuals aged 18 and above, encompassing both men and women, presenting clinical symptoms indicative of SAPS.
The condition incorporates diagnostic labels such as rotator cuff tendinopathy, painful arc syndrome, subacromial bursitis, shoulder impingement, rotator cuff tendinosis or tendinitis, and contractile dysfunction.
Exclusion Criteria:
Participants treated surgically or exhibiting frozen shoulder, post-traumatic shoulder pain, post-traumatic rotator cuff tear, shoulder instability, shoulder osteoarthritis, rheumatoid diseases, neck pain, cancer, neuropathic pain, and neurological conditions were excluded from consideration.

Frozen shoulder
Intervention
Authors included studies involving manual therapy (e.g., joint mobilisation, manipulation, soft tissue mobilisation, or massage) combined with diverse exercises (stretching, range of motion, stabilisation, strengthening, proprioceptive, postural, motor control, or their combinations). These interventions were applied either independently or as additional strategies for adult patients with SAPS.
Comparison
Included studies involved comparisons of corticosteroid injections (guided or unguided), either administered independently or in conjunction with other conservative interventions.
Results
7 studies included in the quantitative synthesis conducted direct or indirect comparisons between EMT and corticosteroid injections.
The meta-analysis results indicated no differences between EMT and corticosteroid injections across very short, short, mid, and long-term durations.
Likewise, four studies assessed pain intensity using either a VAS or NRPS, revealing no differences between EMT and corticosteroid injections in very short, short, and long-term outcomes.

Flow chart of the study

Discussion
Authors conducted an analysis of eight Randomised Controlled Trials involving 946 participants, with a mean age of 53.8 years. All studies exhibited either 'high' (7 trials) or 'moderate' (1 trial) methodological quality.
The primary outcome of our review indicates that an EMT-based treatment approach demonstrates comparable effects in alleviating pain, enhancing function, and promoting self-perceived recovery, when compared to corticosteroid injections across all follow-up durations. However, the quality of evidence ranges from very low to moderate.
The addition of manual therapy to exercises is deemed effective in reducing pain and disability, particularly in the short term, supported by moderate and high levels of evidence. Nonetheless, the effect sizes for EMT compared to control conditions are characterised as small to moderate.

Despite our findings suggesting no discernible difference between EMT and corticosteroid injections across all outcomes and follow-up periods, the certainty of the evidence was downgraded, primarily due to significant clinical and statistical heterogeneity.
The manual therapy approaches varied considerably among eligible studies in terms of type (e.g., glenohumeral and scapular mobilisations, specific soft tissue mobilisation, passive shoulder mobilisation, manual stretching, etc.), number of sessions (6 to 12), and treatment duration (4 to 18 weeks).
Eligible trials employed a diverse range of exercises, encompassing strengthening, stabilization, stretching, and proprioception training programs.
However, the optimal exercise dosage, including total repetitions, sets, number of exercises, frequency, intensity, and duration, was not clearly defined across the studies.
Limitations
Participant differences:
The interpretation of our study findings is influenced by limitations, particularly the heightened clinical heterogeneity present in specific interventions, healthcare practitioners, and patients' characteristics, including symptom duration among the included studies.
Influence on Estimations:
The comparison involving EMT alone or in conjunction with a multimodal physiotherapy program could potentially impact precise estimations, contributing to variability in outcomes.
Recommendations for Future Studies:
To enhance clarity and reliability in research, future studies should meticulously describe all aspects of interventions, including the specific manual therapy techniques, loading interventions, the number of exercises employed, and criteria for treatment progression.
Clinical implications
Individualised Treatment Plans:
Tailor interventions, including manual therapy and exercise, to the individual patient's presentation and response, considering factors such as specific symptoms, functional limitations, and overall health status.
Manual therapy can have pain relieving affects for a period of time, thus, using techniques before rehab session can improve patients satisfaction, help reach further ranges and help with adherence
Corticoid injections should only be considered if conservative treatment has no affects after 12-24 weeks
Regular Monitoring and Reassessment:
Implement regular monitoring and reassessment of patients throughout the treatment course to gauge progress, modify interventions as needed, and ensure timely adjustments to the management plan.
Patient Education and Empowerment:
Emphasise patient education on the nature of Subacromial Pain Syndrome (SAPS), the rationale behind chosen interventions, and the importance of active participation in rehabilitation. Empower patients with self-management strategies for long-term well-being.
Address Psychosocial Factors:
Recognise and address psychosocial factors that may contribute to SAPS, such as stress, anxiety, and fear-avoidance behaviours. Incorporate strategies to enhance psychological well-being and resilience.
Thank you for reading this weeks edition!
Have a browse through our articles to sharpen you diagnostic skills

Reply