- Sports Med U Newsletter
- Posts
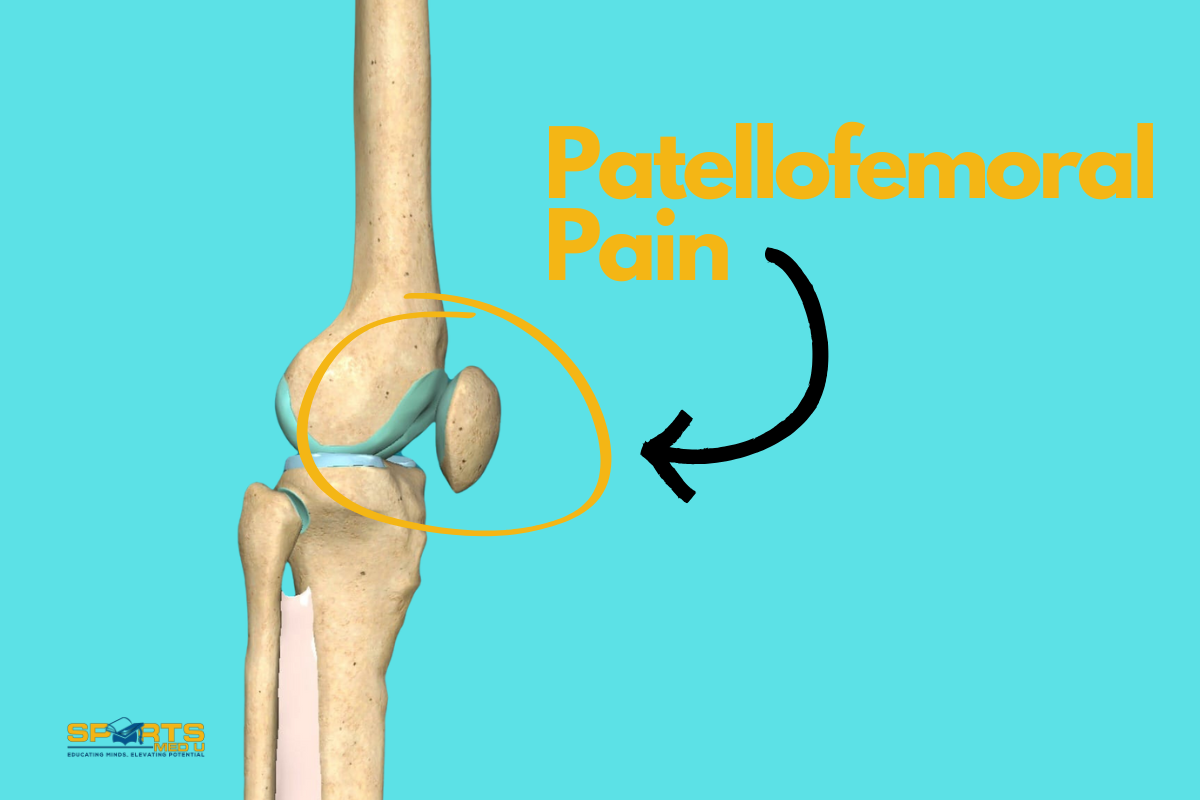
- PFP pain & Alignment - 4 Takeaways
PFP pain & Alignment - 4 Takeaways
Sports Med U | Educating Minds, Elevating Potential
Current concepts in the management of patellofemoral pain — The role of alignment
Stephen, J., Ephgrave, C., Ball, S. and Church, S., 2020. Current concepts in the management of patellofemoral pain—the role of alignment. The Knee, 27(2), pp.280-286.
In today’s letter
4 takeaways from the study looking at PFP and alignment
A fun infographic based from the study!
Rapid Results =
At its core, PFP rehabilitation is a puzzle. The body’s movements are the result of co-ordinated interaction between muscles, joints , and tendons.
Even small deviations in alignment can have ripple effects to force distribution, altering how muscles work and increasing strain.
Retraining movement patterns to optimise muscle efficiency and reduce joint loading, can improve function and decrease injury risk.
3 resources to check out to further your knowledge about patellofemoral pain
Meme of the week: Mmm, not today 💪
Bite-size study - Infographic style!

4 Takeaways
Aim of the study
The study aims to improve rehabilitation for patellofemoral pain (PFP) by discussing:
Movement patterns
Muscle function
Skeletal alignment
To reduce pain and improve functional outcomes
The Rehab Process
In rehabilitation for patellofemoral pain (PFP), the approach starts with correcting movement patterns at the hip, followed by the knee and ankle.
This proximal-to-distal strategy is grounded in the understanding that changes in the alignment and function of the hip can influence the biomechanics of the knee and ankle. The hip is importnat as it controls the lower limb’s alignment during functional movements.
For example, addressing hip extension, abduction, and external rotation can help optimise lower limb function and reduce the load on the patellofemoral joint (PFJ).
The rehabilitation begins with simple, isolated movements to correct the basic muscle actions and prevent compensatory patterns, such as overuse of the tensor fasciae latae (TFL) or improper loading at the knee.
The TFL connects to the IT band and hence can distribute load to the outside of the patella
After focusing on:
Stability
Control
Co-ordination
From a safe perspective a gradual transition to more complex movements patterns that involve the entire kinetic chain, like squatting or lunging can start.
This gradual progression helps ensure that patients develop motor control and avoid returning to harmful movement habits that might exacerbate their symptoms.

Body Map Technique
The body map technique is an effective method to enhance patient awareness of their muscle activation during exercises. After teaching patients the correct movement patterns in a controlled clinical setting, you can ask them to visualise the area where they feel the muscles working during the exercise.
This helps reinforce the connection between the correct muscle activation and the movement pattern, helping patients practice these exercises correctly at home.
Interestingly, this approach also correlates well with the muscles that should be activated based on clinical assessment. It provides immediate feedback to patients, allowing them to self-correct if they’re not feeling the intended muscles engage.
This technique is cost-effective and efficient alternative to expensive and complex diagnostic tools like electromyography (EMG), which has limitations.
Treat The Person, Not The Condition
Personalised rehab in managing PFP, particularly when considering factors like anatomical variations and psychological influences is absolutely key.
For instance, patients with increased femoral anteversion—an abnormality in the rotation of the femur—may experience difficulties in correctly engaging muscles during rehab, such as the gluteus medius.
This anatomical factor can make it harder for them to perform hip abduction and extension, leading to suboptimal muscle activation.
Additionally, the study notes that psychological factors, such as fear of pain or anxiety, can significantly impact patient outcomes. These factors can lead to muscle guarding or avoidance behaviours, which in turn hinder the progress of rehabilitation.
Therefore, recognising the persons differences in anatomy and addressing psychological barriers is the first of many steps.

Biomechanical Principles
This study highlights how important it is to consider biomechanics when designing rehab programs for people with PFP. To create effective treatments, it’s key to understand how muscles work together, how joints align, and how forces impact the patellofemoral joint (PFJ).
Moving well doesn’t just lower the risk of injury; it also makes muscles work more efficiently by activating the right ones at the right time. Even small alignment changes in the pelvis, hip, or legs can significantly affect how forces are spread across the joints, which can worsen PFP symptoms.
For instance, poor pelvic alignment can strain the knee and change how muscles like the glutes or quads function.
Clinical Tip
Checking for compensations:
Observing how patients perform tasks such as hip abduction or extension can show whether they’re compensating with other muscles or positioning their joints in awkward angles.
For example, excessive hip flexion during abduction might signal that the TFL is overcompensating for weak glutes, increasing lateral patellar stress.

Top 3 Resources to Check Out
And learn more about PFP
A deep dive into PFP diagnosis and management - By yours truly 🙂
Rehab leaflet for patients - (PDF) - LINK 🤓
Body mapping explained - (Video)
Meme of The Week

Thank you for reading this weeks edition!
Have a browse through our articles to sharpen you diagnostic skills

Reply