- Sports Med U Newsletter
- Posts
- The Brain & Ankle Sprains 🧠
The Brain & Ankle Sprains 🧠
Sports Med U | Educating Minds, Elevating Potential
Brain Neuroplasticity Related to Lateral Ankle Ligamentous Injuries: A Systematic Review
Maricot, A., Dick, E., Walravens, A., Pluym, B., Lathouwers, E., De Pauw, K., Verschueren, J., Roelands, B., Meeusen, R. and Tassignon, B., 2023. Brain neuroplasticity related to lateral ankle ligamentous injuries: a systematic review. Sports Medicine, 53(7), pp.1423-1443.
In today’s letter
Overview of how the brain is affected post lateral ankle sprains
How to apply all of this nitty gritty into practice
Resources to delve deeper and learn more about the ankle 🧠
Rapid Results =
Patients with chronic ankle instability or a history of lateral ankle sprains show real neurological adaptations. Meaning their brain changes how it communicate with ankle muscles.
Professional takeaway =
Start proprioception, neuromuscular control, dual-tasking, and even explosive exercises early.
Definitions Simplified
Let’s simplify the jargon so your eyes don’t glaze over:
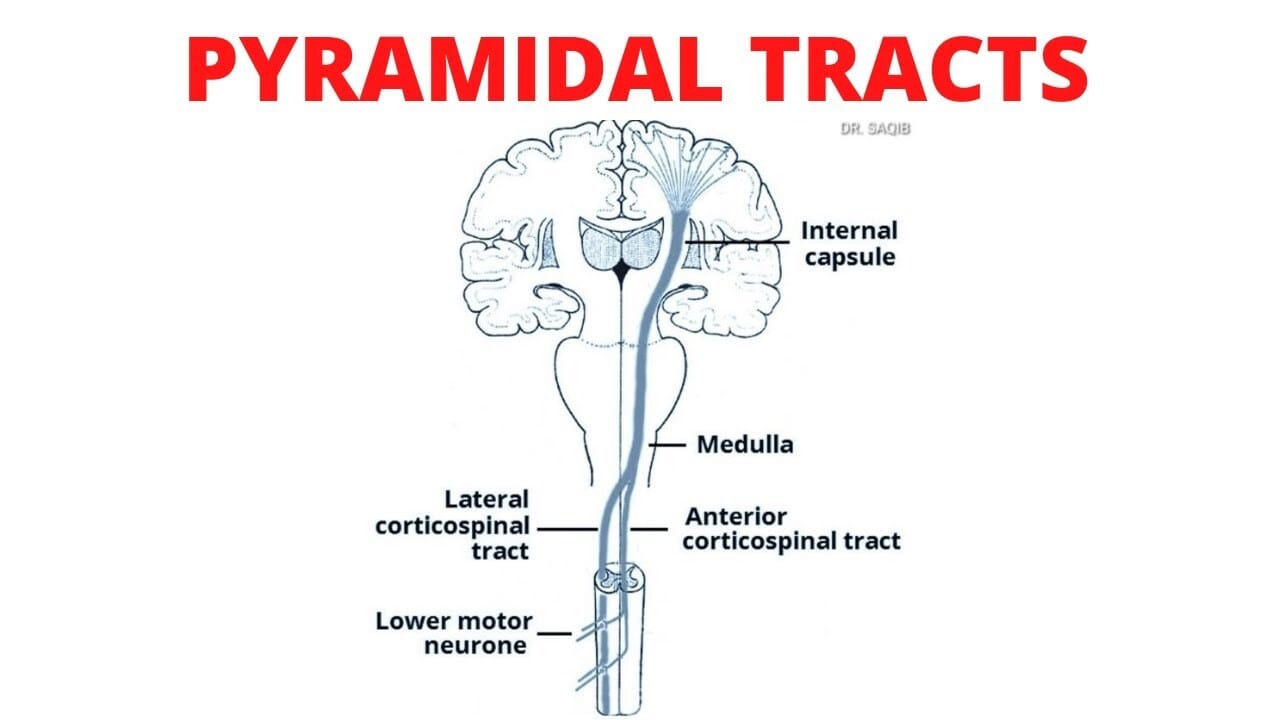
Corticomotor excitability → How easily the brain’s motor cortex can fire signals to make muscles move.
Corticospinal inhibition → When the brain tells certain motor pathways to “slow down” or hold back.
Corticomotor output mapping → A brain map showing which parts control specific muscles.
Postcentral gyrus → Brain region that processes sensory input from the body, like touch and position.
Afferent information → Sensory signals traveling from the body to the brain.
Somatosensory cortex → Processes all that sensory input so you know where your body is in space.
Afferent information decoupling → When sensory signals get “scrambled” or reduced after injury.
Transcranial magnetic stimulation (TMS) → A way to poke the brain with magnets and see how it reacts.
Cortical silent period → Short pause in brain activity after a muscle fires; tells us about inhibition in the motor system.

Deeper look
Aim of the study
To determine if ankle sprains and chronic ankle instability cause changes in brains signalling, cortical mapping, or neuroplasticity
Did you know?
Ankle sprains are a pretty common occurrence in professional & recreational athletes, occurring at a rate of 11.3 per 1,000 exposures.
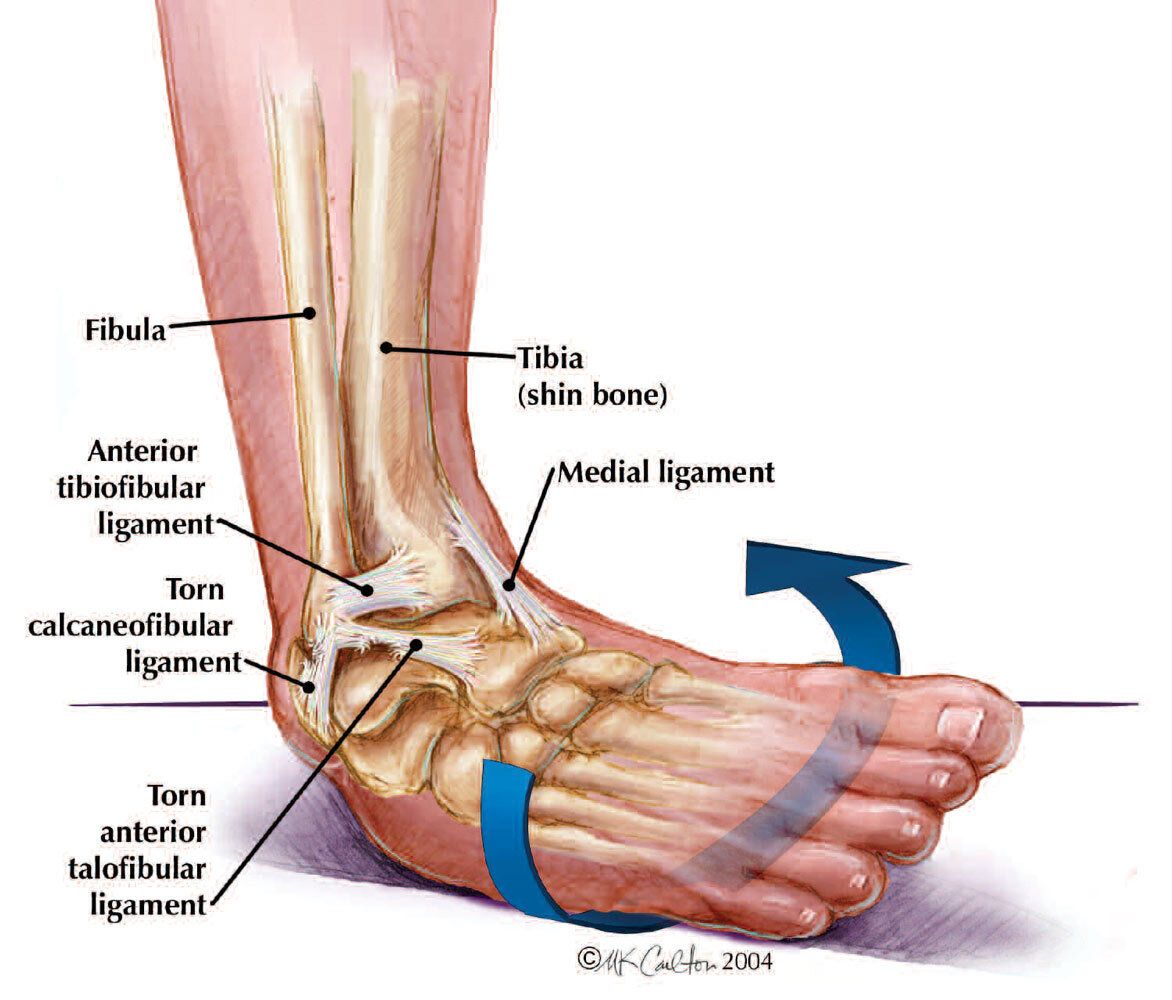
It typically damage ligaments, but can also affect muscles, and nerves, which leads to swelling, and reduced neuromuscular activation.
While most ankle sprains heal with time, some patients develop chronic ankle instability (CAI), a condition that can last for a year or longer. Those with CAI often experience a persistent sense of instability, avoid certain activities, and see a higher risk of repeated ankle sprains
Research indicates (this one included) that after a simple ankle roll there can be significant changes in the central nervous system (the brain and spinal cord), which partially explain why these re-injuries are so common.
Methods
This systematic review analysed 20 articles that looked into:
356 patients with chronic ankle instability
10 people with recent lateral ankle sprains
46 “copers” - people who had experienced at least one ankle sprain but recovered fully without ongoing dysfunction.
The focus of the review was strictly on brain structure and function, excluding studies involving animals, cadavers, unrelated injuries, or treatments that did not address neuroplasticity.
Results
The review found that patients with CAI displayed lower corticomotor excitability, particularly in muscles responsible for stabilising the ankle, such as the peroneus longus and tibialis anterior.
Corticospinal inhibition was also higher, indicating that the brain exerts greater suppression on muscle activation, as evidenced by longer cortical silent periods.
Furthermore, corticomotor output maps were smaller and more concentrated, showing that fewer neurons were dedicated to controlling main ankle muscles in CAI patients compared to healthy people or copers.
Refer to definitions to help you make sense of all the technical terms 😉

The Affect Of Ankle Sprains In More Detail
Okay, buckle up boys and girls. The study uses a lot of complicated words, but I did my best to break this down and simplify it as much as possible
Functional Brain Adaptation
Corticomotor excitability reflects how easily neurons in the motor cortex fire to activate muscles.
In patients with chronic ankle instability, studies consistently show reduced excitability in areas of the primary motor cortex that control leg muscles, such as:
Peroneus longus
Tibialis anterior
Soleus
Medial head of gastrocnemius
This means that communication along the pyramidal tracts is less efficient, which may contribute to activation deficits, particularly in postural control.
Smaller corticomotor map areas and volumes suggest that neurons are more tightly clustered when communicating with the peroneus longus, leaving fewer neurons available for flexible control.
As a result, some motor cells that normally support the peroneus longus are less dedicated to its function, while other brain regions step in to compensate.
This shift in muscle excitability may underlie the altered movement patterns seen in CAI, ultimately increasing the risk of ankle re-injury.
Brain’s Understanding of Sensory Information
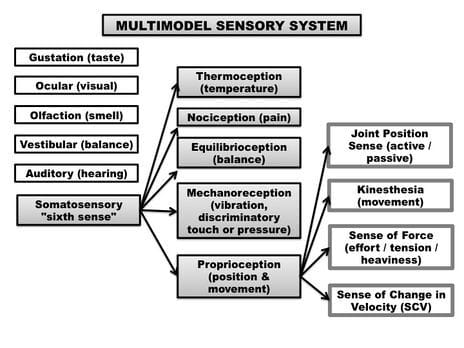
Proprioceptive feedback, which refers to the signals your brain receives from your foot about position and movement, is also altered in CAI
Research suggests that changes in the postcentral gyrus reduce how well sensory information is integrated. As stimulus intensity increases, this disruption becomes more pronounced, potentially limiting the brain’s ability to anticipate or respond to movement.
Since the somatosensory cortex is important in interpreting proprioceptive input, changes in this area can alter joint perception and reduce awareness of ankle position.
Altered somatosensation can therefore directly influence movement patterns, postural control, and just general injury risk.
Fear
Fear of reinjury is another factor in the disability experienced by patients with lateral ankle sprains (LAS).
One study looked into brain activity during injury-related movements, such as simple direction changes, and found significant deactivation in the dorsal anterior cingulate cortex (limbic region associated with increased fear levels)
This means that patients with LAS experience more anxiety when exposed to sprain-related stimuli compared to healthy people.
Over time, this initial avoidance response can become maladaptive. Patients may begin to avoid sports or physical activity altogether due to fear of re-injury, which in turn reinforces functional limitations and reduces overall participation.
Structural Brain Adaptation
Past the functional changes, structural adaptations in the brain also appear to occur in CAI.
Evidence suggests alterations in the corticospinal tract, indicating that electrophysiological changes are accompanied by measurable structural modifications.
Or in more simple terms, there are changes in nerve communication and the physical structure of the corticospinal tract, which carries movement signals between the brain and muscles
These injuries may also lead to changes in white matter microstructure, which is important for postural control.
If left unaddressed, such structural alterations could increase the risk of future injuries of the lower limb.
3 Clinical Tips
The neural adaptations can result in compensatory movement patterns, and persistent pain. Copers, in contrast, show minimal or no significant brain changes. Rehabilitation should therefore target both the brain and the ankle.
Proprioceptive training can help retrain the brain to accurately sense and respond to ankle position, while balance and motor learning exercises improve movement patterns.
Addressing fear of reinjury is critical, and questionnaires such as the Injury-Psychological Readiness to Return to Sport Scale can help clinicians assess readiness and encourage safe, confident return to activity
Top Resources to Check Out
And learn more about ankle sprains
Simple Ankle Sprain Guidelines (pdf) —> LINK 🦶
Lecture on CAI & LAS
Meme of The Week

When You’re Ready to Learn More
We have great resources for you to devourer
Killer Articles —> Literally everything you need to know about a specific injury
Tendinopathy 4 phase rehab frame work - My book that walks you through a step by step process of treating tendons
Tendininopathy Specific Guides - Learn how to diagnose, manage & treat patellar, achilees and shoulder tendinopathies

Reply